Background
- First performed in New Zealand in 1997.
- Dr. James Lingeman (IU Health) brought HoLEP to the United States in 1999.
- Multiple studies cite HoLEP as the new gold standard for BPH.
- Per updated 2018 AUA guidelines, laser enucleation of the prostate is the ONLY size-independent surgical intervention for enlarged prostate (i.e. BPH or benign prostatic hyperplasia).
Indications
- Kidney function decline secondary to BPH.
- Urinary retention secondary to BPH.
- Recurrent urinary tract infections (UTls).
- Recurrent bladder stones or gross blood in the urine due to BPH.
- Lower urinary tract symptoms (LUTS) attributed to BPH refractory to and/or unwilling to use other therapies.
- HoLEP particularly helpful for prostates 80 g or larger since other therapies are less effective.
- HoLEP helpful in men whose bladders have poor function as studies have shown men can typically still empty without a catheter even if the bladder does not work well, 50% chance of voiding without a catheter with little to no bladder function (voiding is accomplished by Valsalva/bearing down).
- HoLEP useful in men with large prostates who have elevated PSA and prior negative biopsy because removes a large amount of tissue which is sent as a large biopsy, and after surgery expect PSA to be low around one or less and if not a repeat biopsy should be more diagnostic.
Operation
- Anesthesia: general.
- Duration: typically 2-3 hours depending on size of prostate and anatomy.
- All endoscopic except one out of 200 cases where prostate tissue does not morcellate and a lower abdominal incision has to be made to open the bladder and remove the tissue, but an alternative to that is to run saline irrigation into the bladder overnight which typically softens the tissue and then repeat morcellation the day after surgery.
- Awaken from surgery with a foley catheter in place with saline irrigation running through it to wash any old blood or debris out from the surgery. The catheter has a large balloon which helps control bleeding from the prostate as well.
Hospitalization
- Typically outpatient admission for observation (< 24 hours), keep patients overnight to monitor for bleeding and make sure catheter does not clog by running irrigation through it.
- Check postoperative labs (blood counts, electrolytes, kidney function) as a precaution.
- Once fully awake can eat/drink, can walk with nurses assistance.
- On day after surgery as long as you are doing well, the nurses remove the catheter around 4-Sam in order to allow time for you to urinate. If the nurses have any concerns, they wait for me to see you in the morning before removing the catheter.
- With the catheter out, we ask that when you void you use a hand-held urinal so we can measure the volume voided and assess the color of the urine which gives an indication on how much bleeding there is. Typically, at least two bladder scans with relatively low volumes and good voided volumes meets discharge criteria.
- 90% of patients are discharged home on the day after surgery without a catheter.
Outcomes
- 2% complication rate - bleeding (blood transfusion or clot retention), infection (UTI), injury to nearby structures (urethra/bladder).
- Blood in the urine normal/expected postop, improves with time. If on blood thinners can take weeks/months to resolve.
- Burning with urination is common due to the raw surface in the prostatic urethra from the surgery and resolves with time, sometimes in days but can take weeks/months in some men.
- Urethral stricture/bladder neck contracture/regrowth of prostate requiring treatment 1-2%.
- Short term stress and/or urge incontinence 25-30%, long term 1%.
- Stress: the urethral sphincter is a muscle that sits below the prostate and is responsible for continence.
This muscle is weakened in men with large prostates because the prostate has limited the amount of lifting this sphincter has had to do to hold back the urine (prostate is an upstream dam). Once the prostate size is largely reduced, the sphincter has to do more work and is atrophy is significant there can be leakage until the pelvic floor regains strength. - Urgency: some patients get frequency/urgency after this operation. The bladder for years has had to squeeze very hard to get urine past the prostate. After the surgery, the bladder does not need to do this because the obstruction is gone, but the bladder nerves need time to adjust to this. Nerves heal slowly so this process can take several months.
- On average, any postoperative urinary symptoms are improving by three months, only 1% chance the incontinence lasts more than one year.
- Stress: the urethral sphincter is a muscle that sits below the prostate and is responsible for continence.
- 90% chance of retrograde ejaculation
- Could be diminished or absent ejaculated with orgasm/climax, not harmful, semen will go back into the bladder but then with the next void will empty in the urine.
- Semen enters urethra below the prostate and after prostate surgery the path of least resistance is to go back into the bladder instead of out the small urethral channel.
- Nerves that control erections are outside the prostate and not affected by the surgery, so erectile function does not typically change.
Less than 10 percent chance of incidental prostate cancer identified on pathology. This surgery does not preclude other treatments (radical prostatectomy, radiation, etc.).
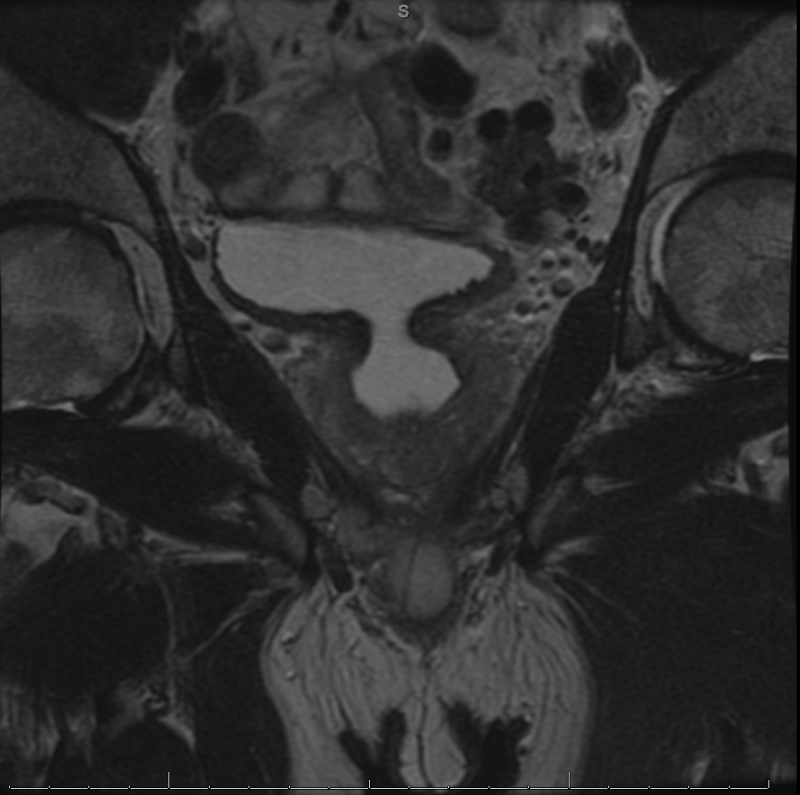
Post-HoLEP shows where the laser removed the transition zone of the prostate to create an open channel with no obstruction of the bladder.
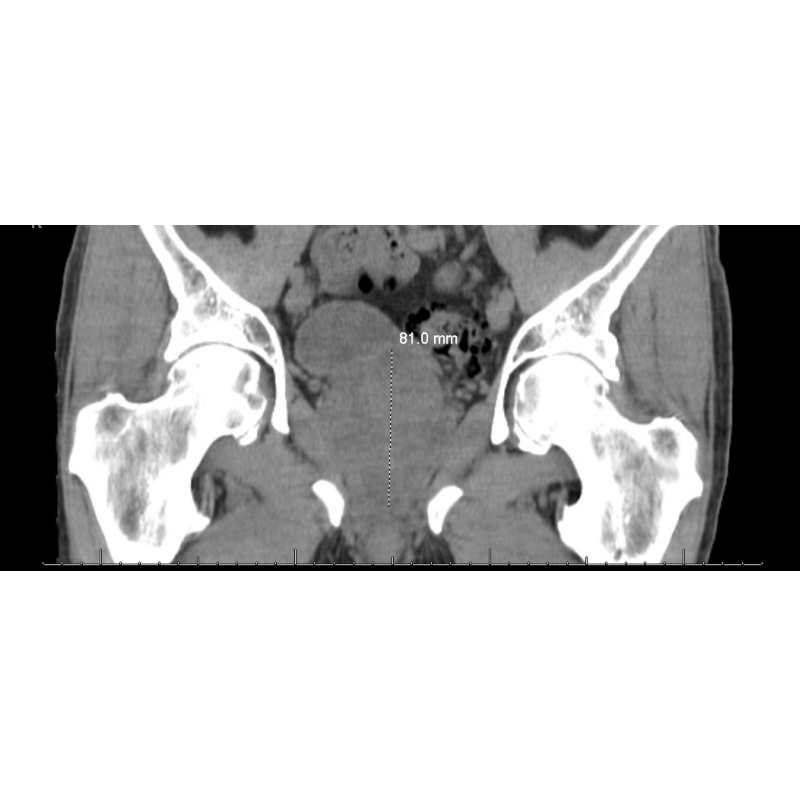
Pre-HoLEP shows enlarged prostate, 8 cm in length, with mass effect on the floor of the bladder and bladder outlet obstruction from the prostate.
Return To Work/activities After Surgery
- Determined on a case by case basis, depends on type of work and if the patient is on any blood thinners.
- Resuming blood thinners is determined on an individual basis.
- Prostate medications are stopped immediately postop.
- In general, one week of light activity postop (no lifting > 15 pounds, no strenuous activity/exercise but normal amounts of walking and stairs are fine), then resume all activity as tolerated after that. If more blood in the urine is seen after a certain activity, recommend waiting a few days and then trying again.
- No straddling objects, bike riding or hot tubs for one month postop.
Follow-up
- You will receive a call with your pathology results, typically takes a few business days.
- Postop visit is typically three months after surgery with a PSA blood test prior.
Durability
- Reoperation for regrowth is 1%.
- A prior study showed at seven years postop, HoLEP 0% reoperation rate vs. 18% for TURP.
- 95% of patients satisfied or very satisfied on survey data at 10 years postop.
 937-293-1622
937-293-1622 Find a Location Near You
Find a Location Near You



